“Living with Chest Pain One Year After Stent Placement: What to Expect”
-
- Dr. Junaid Arshad
- March 17, 2023
- 0 comments
Table of Contents
What Causes Chest Pain Months After Stent Placement?
Chest pain that occurs months to years after stent placement may be a sign of gradually developing blockage in your stent. This phenomenon is not very uncommon and affects 6-20% of the patients who get a stent.[1] In medical terminology, it is called In-stent restenosis (ISR). It is diagnosed by an angiogram & is defined as a decrease in lumen diameter of 50% or more. ISR may be treated with either medical therapy, balloon angioplasty, redo stent procedure & CABG surgery in certain cases. The treatment option varies from patient to patient and is decided after a shared decision between a cardiologist, cardiac surgeon, & the patient.
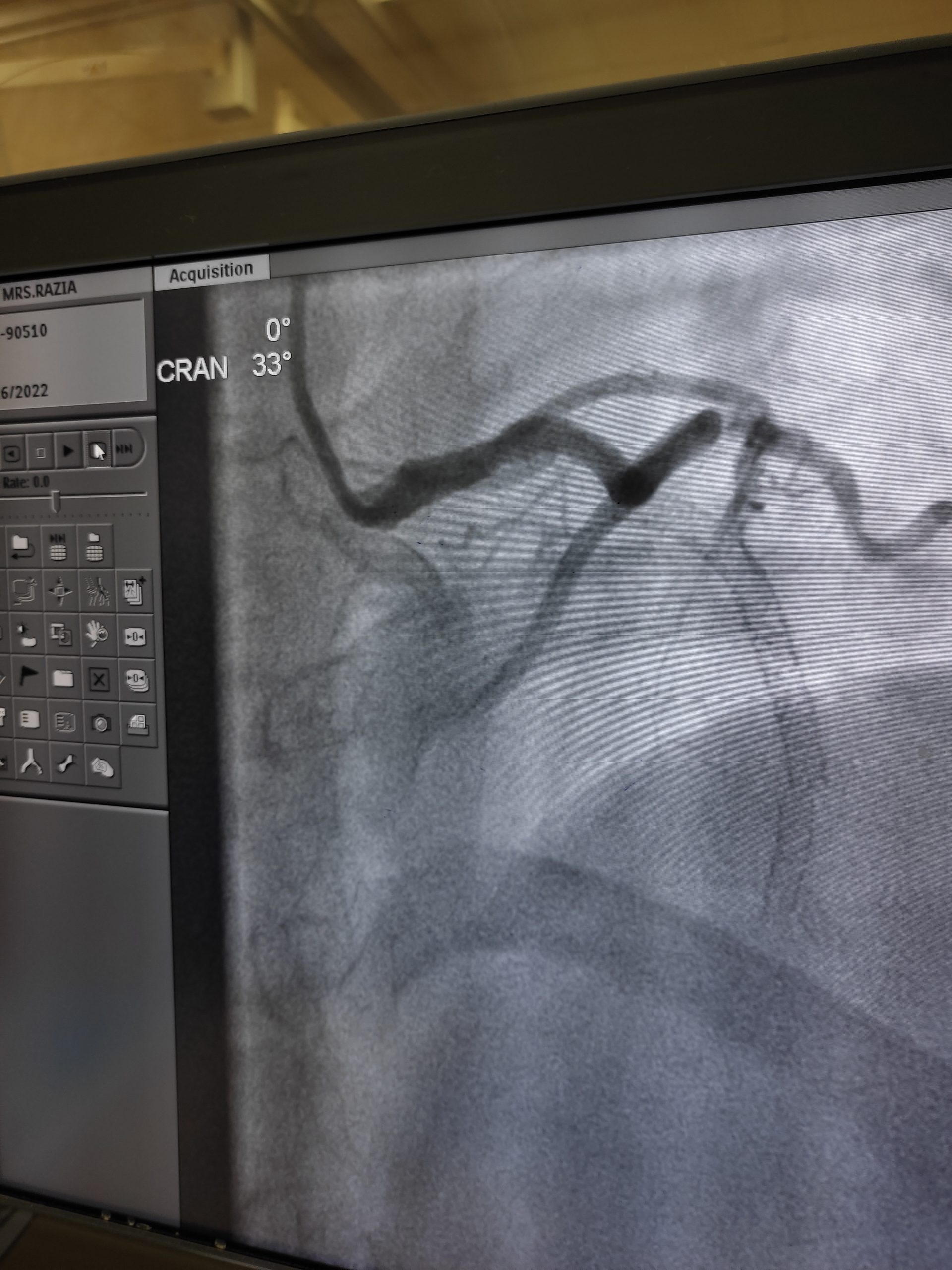
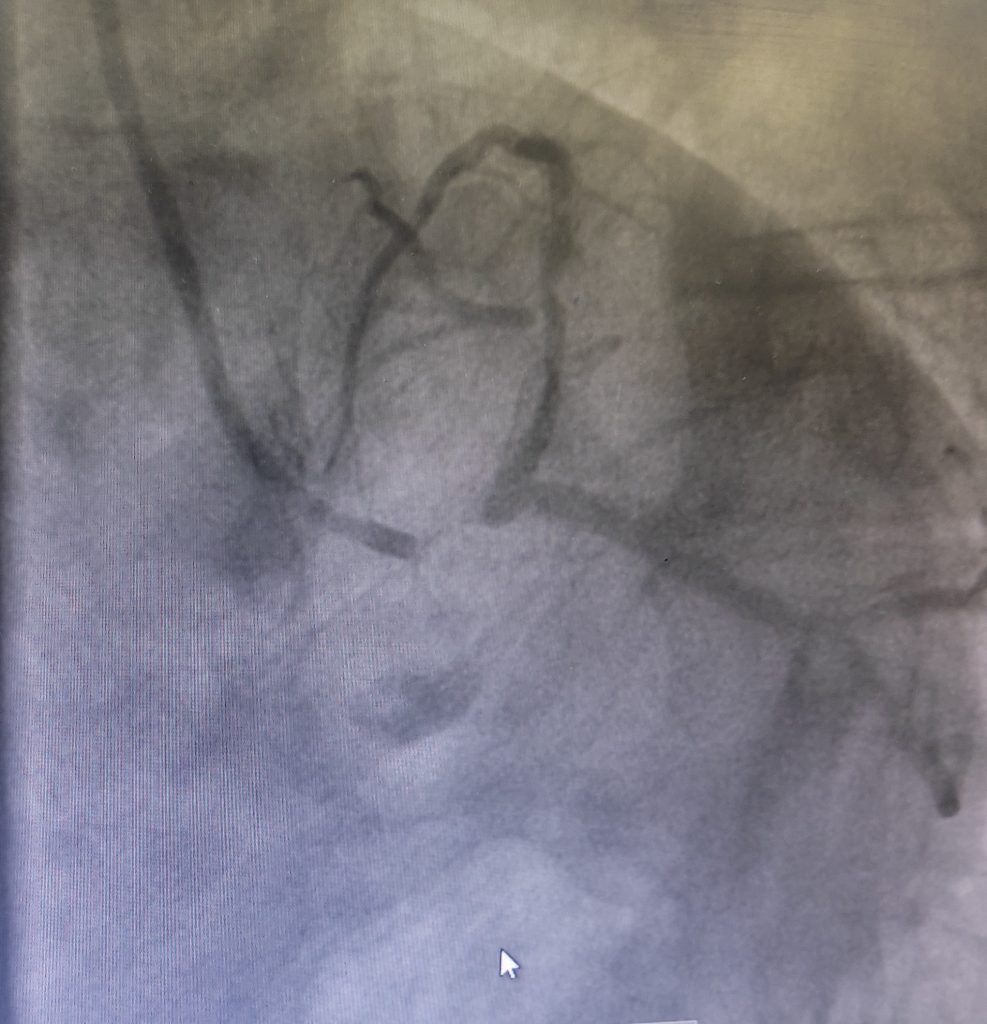
Angiographic Images showing critical left main stem disease and ISR in LAD artery

Given below are further details of ISR and associated conditions.
Mechanisms of ISR
There are several mechanisms that can contribute to ISR:
Neointimal hyperplasia
This is the most common mechanism of ISR.
When a stent is placed in an artery, it can cause injury to the arterial wall.
In response, the body sends cells to the area to repair the damage.
These cells can then multiply and form a layer of tissue over the stent, which is called neointimal hyperplasia.
If this layer becomes too thick, it can narrow or block the stent.
Inflammation
Inflammation can also contribute to ISR.
When a stent is placed in an artery, it can cause an inflammatory response in the body.
This can lead to the release of chemicals that can cause the arterial wall to thicken and narrow.
Elastic recoil
Elastic recoil is when the arterial wall contracts after the stent is deployed, which can cause the stent to become narrowed.
This can happen if the stent is not properly sized for the artery or if the stent is not fully expanded during the procedure.
Late-acquired malapposition
This is when the stent becomes partially or fully detached from the arterial wall. This can happen if the stent is not properly positioned or if the arterial wall changes over time.
Symptoms of ISR
The symptoms of in-stent restenosis may vary depending on the severity of the condition and can include:
Chest pain (angina)
This is the most common symptom of in-stent restenosis.
It can occur during physical activity or at rest.
The patient experiences chest pain, heaviness, or tightness that may be referred to left arm or back.
It may also be accompanied by apprehension and sweating and lasts from 2-20 minutes.
For more detailed features of heart-related chest pain check out this detailed article. Click here
Shortness of breath
This can occur due to the reduced blood flow to the heart muscle, which can cause the heart to work harder to pump blood.
Fatigue
Reduced blood flow to the heart muscle can cause the heart to work harder, leading to fatigue.
Sweating
Excessive sweating can be a symptom of in-stent restenosis, especially during physical activity.
Nausea or vomiting
These symptoms can occur due to reduced blood flow to the digestive system.
Dizziness or lightheadedness
Reduced blood flow to the brain can cause these symptoms.
Diagnosis of ISR
To diagnose ISR, doctors may use different imaging techniques.
One common method is coronary angiography, where a thin tube is inserted into the artery and a special dye is injected.
This allows the doctor to see any blockages or narrowings in the artery, including those that occur within the stent.
Another method is intravascular ultrasound (IVUS), where a tiny ultrasound probe is inserted into the artery to produce images of the inside of the vessel.
This can provide detailed information about the stent and any blockages or narrowings.
Optical coherence tomography (OCT) is a newer imaging technique that uses light waves to produce high-resolution images of the artery.
This can provide very detailed information about the stent and any blockages or narrowings.
Fractional flow reserve (FFR) is a test that measures the pressure difference across a blockage in the artery. This can help doctors determine whether a blockage is causing a significant reduction in blood flow and whether further intervention is necessary.
Cardiac magnetic resonance imaging (MRI) is another imaging technique that can provide detailed images of the heart and blood vessels. However, this is less commonly used for diagnosing ISR.
In summary, there are various imaging techniques that can be used to diagnose in-stent restenosis.
The choice of technique depends on the individual case and the resources available, but coronary angiography is the most common and reliable method.
Prevention of ISR
Here are a few strategies that can help prevent ISR post-angioplasty:
Medication compliance
Taking prescribed medications as directed is essential to prevent ISR.
Medications like aspirin, clopidogrel, statins, ACE inhibitors, or ARBs can reduce the risk of restenosis.
It is crucial to take these medications regularly and as directed by your doctor.
Lifestyle modifications
Making healthy lifestyle choices can help reduce the risk of ISR.
Quitting smoking, maintaining a healthy weight, following a healthy diet, and engaging in regular physical activity can help prevent the recurrence of cardiovascular disease.
Close monitoring
Regular follow-up visits with your doctor are essential to detect and treat any signs of restenosis early. Your doctor may recommend routine angiograms or other imaging tests to monitor the stented artery’s health.
Drug-eluting stents
Using drug-eluting stents (DES) during angioplasty can reduce the risk of ISR.
These stents are coated with medications that are slowly released into the surrounding tissue, reducing the likelihood of restenosis.
Radiation therapy
In some cases, your doctor may recommend radiation therapy to prevent ISR.
This therapy involves using high-energy radiation to reduce the risk of restenosis.
In summary, preventing ISR post-angioplasty involves medication compliance, lifestyle modifications, close monitoring, the use of drug-eluting stents, and in some cases, radiation therapy. It is essential to work closely with your doctor to develop a personalized treatment plan to reduce the risk of restenosis and promote a successful recovery.
Stent Thrombosis
Another possible cause of chest pain after stent placement is thrombosis or blood clotting within the stent.
This usually happens when the patient stops taking their prescribed antiplatelet medication, which helps prevent blood clots from forming.
Blood clots can obstruct the stent, causing chest pain and other symptoms.
If a blood clot is suspected, urgent medical attention is required to prevent serious complications such as heart attack or stroke.
The difference between stent thrombosis and ISR is that of time duration.
Stent thrombosis usually develops more acutely and can mimic the picture of an acute massive heart attack.
Whereas ISR develops gradually over time and the patient experiences anginal symptoms or shortness of breath.
Overall, while both stent thrombosis and stent restenosis can be serious complications of stent placement, they have different underlying causes and treatments.
It’s important to take steps to prevent both of these complications, such as taking medications as prescribed and making healthy lifestyle changes.
References
- Li M, Hou J, Gu X, Weng R, Zhong Z, Liu S. Incidence and risk factors of in-stent restenosis after percutaneous coronary intervention in patients from southern China. Eur J Med Res. 2022 Jan 22;27(1):12. doi: 10.1186/s40001-022-00640-z. PMID: 35065663; PMCID: PMC8783476.




